You’re probably reading this because your dentist or endodontist has said you have a diseased or injured tooth. If so, rest assured that in the majority of cases, your tooth can be saved with endodontic treatment. Sometimes, however, a tooth cannot be saved, and will need to be extracted and replaced with a prosthetic, or artificial, tooth. This section explains the treatment options available to you, so that you can discuss them with your dentist or endodontist and make the best choice for your needs.
Treatment Options for the Diseased Tooth
- What’s happening to your tooth?
- How does endodontic treatment save the tooth?
- What is retreatment?
- What is endodontic surgery?
- What are alternatives to endodontic treatment?
- Dental Implants vs. Root Canal Therapy
What’s happening to your tooth?
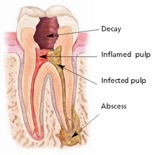
To understand treatment options for your diseased tooth, it helps to know about the anatomy of the tooth. Inside the tooth, under the white enamel and a hard layer called the dentin, is a soft tissue called the pulp. The pulp contains blood vessels, nerves and connective tissue, and helps to grow the root of your tooth during development. In a fully developed tooth, the tooth can survive without the pulp because the tooth continues to be nourished by the tissues surrounding it.
Endodontic treatment – also known as a root canal – treats the inside of the tooth. Endodontic treatment is necessary when the pulp becomes inflamed or infected. The inflammation or infection can have a variety of causes: deep decay, repeated dental procedures on the tooth, faulty crowns, or a crack or chip in the tooth. In addition, trauma to a tooth may cause pulp damage even if the tooth has no visible chips or cracks. If pulp inflammation or infection is left untreated, it can cause pain or lead to an abscess.
How does endodontic treatment save the tooth?
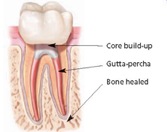
During root canal treatment, the inflamed or infected pulp is removed and the inside of the tooth is carefully cleaned and disinfected, then filled and sealed with a rubber-like material called “gutta-percha.” Afterwards, the tooth is restored with a crown or filling for protection. After restoration, the tooth continues to function like any other tooth.
Contrary to jokes about the matter, modern root canal treatment is very similar to having a routine filling and usually can be completed in one or two appointments, depending on the condition of your tooth and your personal circumstances. You can expect a comfortable experience during and after your appointment.
Saving the natural tooth with root canal treatment has many advantages:
- Efficient chewing
- Normal biting force and sensation
- Natural appearance
- Protects other teeth from excessive wear or strain
Endodontic treatment helps you maintain your natural smile, continue eating the foods you love and limits the need for ongoing dental work. With proper care, most teeth that have had root canal treatment can last as long as other natural teeth and often for a lifetime.
What is retreatment?
As occasionally happens with any dental or medical procedure, a tooth may not heal as expected after initial endodontic treatment for a variety of reasons. These could include complicated canal anatomy that was undetected in the first root canal procedure, the delay in placement of a crown or other restoration, or an insufficient restoration. Sometimes new problems may jeopardize a tooth that was already treated, such as new decay, a loose, cracked or broken filling, or a tooth fracture. Often, when this happens, revision of the previous treatment may be performed to save the tooth.

During endodontic retreatment, the doctor will regain access to the root canal filling material. After removing the canal filling, the doctor can clean the canals and carefully examine the inside of the tooth, searching for any hidden canals or unusual anatomy that requires treatment.
After cleaning the canals, the endodontist will fill and seal the canals and place a temporary filling in the tooth. As with the original root canal, you will need to return to your dentist as soon as possible to have a new crown or other restoration placed on the tooth to protect it.
If retreatment is not an option, endodontic surgery should be considered to save the natural tooth.
What is endodontic surgery?
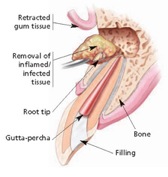
There are many surgical procedures that can be performed to save a tooth. The most common is called an apicoectomy, or root-end resection, which is occasionally needed when inflammation or infection persists in the bony area around the end of your tooth after a root canal procedure. In this microsurgical procedure, the endodontist opens the gum tissue near the tooth to see the underlying bone and to remove any inflamed or infected tissue. The very end of the root is also removed. A small filling may be placed to seal the end of the root canal and few stitches or sutures are placed to help the tissue heal. Over a period of months, the bone heals around the end of the root. Local anesthetics make the procedure comfortable, and most patients return to their normal activities the next day. Postsurgical discomfort is generally mild.
What are alternatives to endodontic treatment?
The alternative to endodontic treatment is extraction of the tooth. Missing teeth can make you self-conscious, affect your ability to bite and chew, cause other healthy teeth to shift and have a negative impact on your overall health. For these reasons, an extracted tooth should be replaced with an artificial one.
Bridges and Removable Partial Dentures vs. Root Canal Therapy
For replacement of an extracted tooth, you may consider a bridge or removable partial denture. These options require additional dental procedures on adjacent healthy teeth, and should be discussed with your dentist or specialist.
Dental Implants vs. Root Canal Therapy
Dental implants have become an important treatment for the replacement of teeth lost due to disease, injury, or congenital tooth agenesis (Adell et al. 1990). Over the past 30 years, the incorporation of dental implants into everyday clinical dental practice has resulted in major improvements in oral health of our patients through enhancements in function, esthetics, and phonetics. [However,] most all dental implant systems are susceptible to peri-implant biological complications (Derks et al. 2015). These complications result in very difficult to treat options, including local mechanical therapy and antibiotics, resective surgery, regeneration, or, in a large number of cases, removal. The erroneous belief of implants yielding a better long-term prognosis has now clearly been rejected in several comparative studies and systematic reviews. Teeth even compromised because of periodontal disease or endodontic problems may have a longevity that surpasses by far that of the average implant.
*Journal of Dental Research jdr.sagepub.com doi: 10.1177/0022034515618942 JDR January 2016 vol. 95 no. 1 5-6 Are Dental Implants a Panacea or Should We Better Strive to Save Teeth? W.V. Giannobile1, 2⇑ N.P. Lang3
